Aetna Reimburses 25% Less Than What They Claim
tl;dr - Aetna says they’ll reimburse 140% of the “Medicare Allowable Rate” for out-of-network medical expenses. In my case they find that number and reduce it by 25%.
Let’s investigate the above statement regarding out-of-network medical reimbursement.
I normally wouldn’t take the time, but after being reimbursed what felt like the wrong number for months (but nearly close enough) I needed to do the math myself.
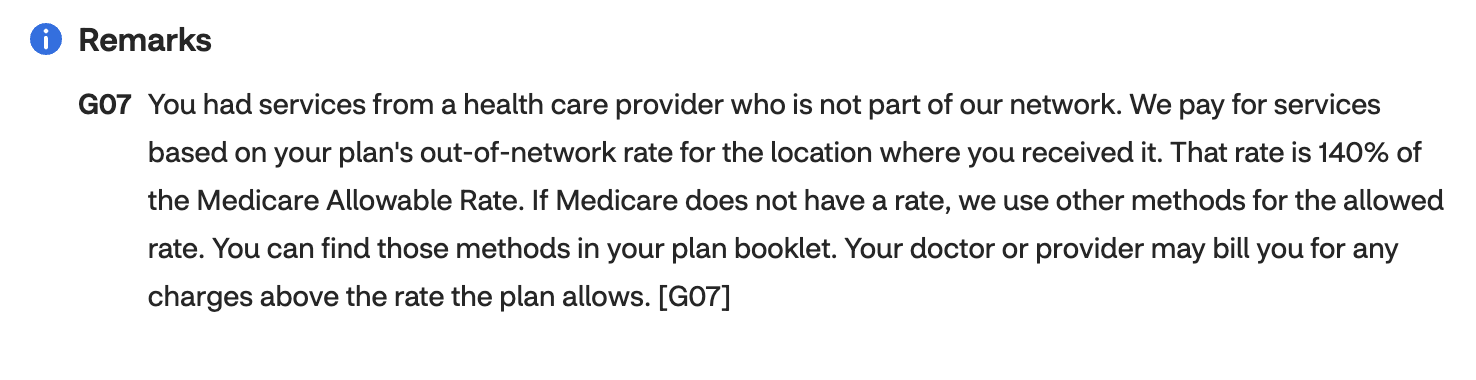
Let’s take a look at this claim:
“We pay for services based on your plan’s out-of-network rate for the location where you received it. That rate is 140% of the Medicare Allowable Rate“
Before we get to what the number actually is, let’s start with what they say it is:
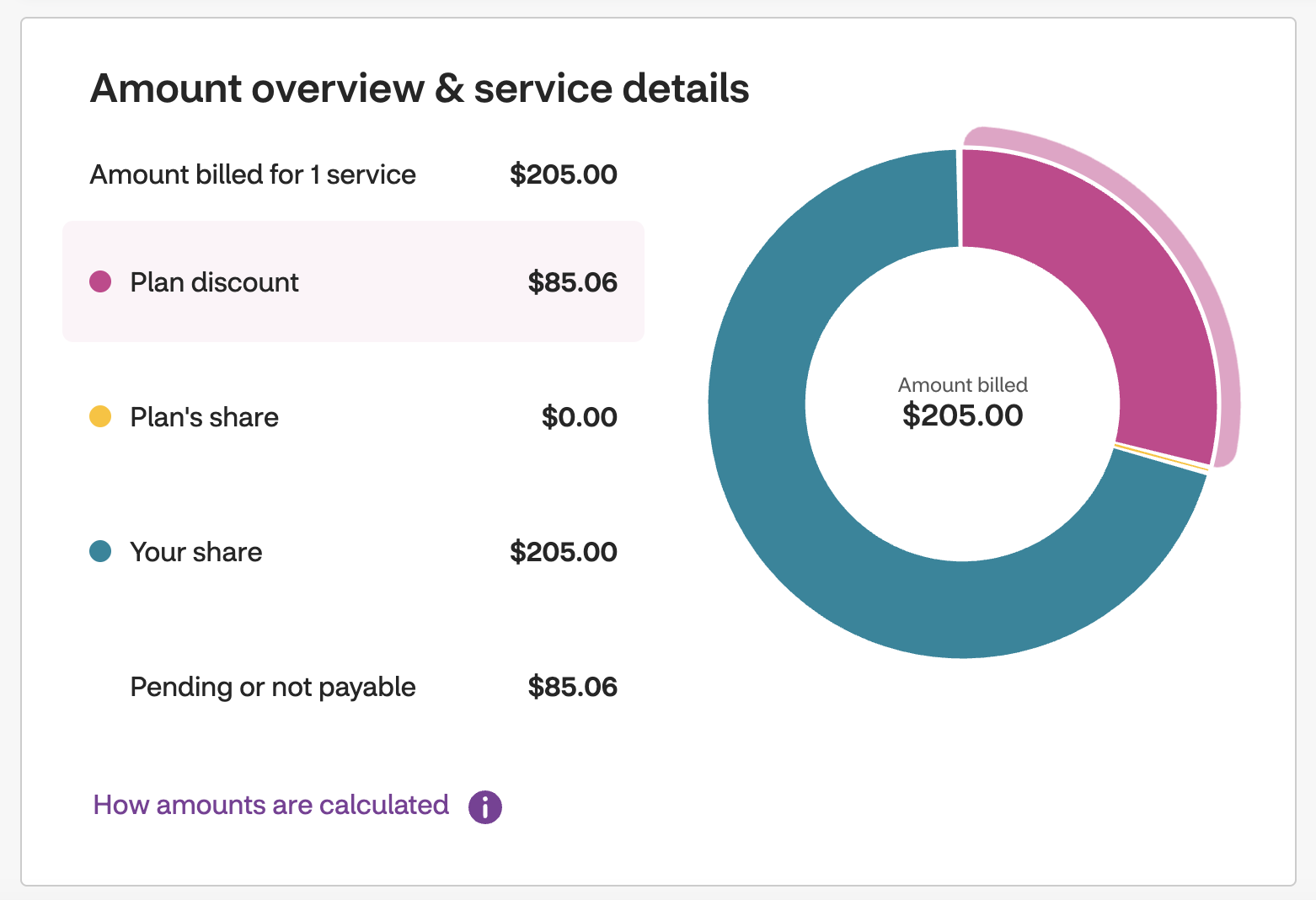
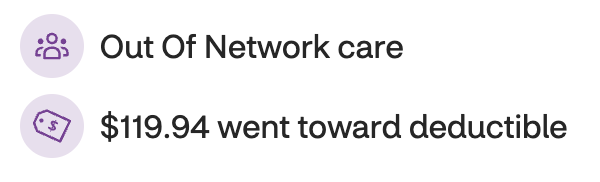
If you do the math ($205-$85.06) you end up with $119.94 which is what went to my deductible.
For 45 minutes of psychotherapy in Manhattan that’s sounding a bit low already. Let’s see what the government thinks you should pay and then apply Aetna’s 140% multiple.
Medicare Allowable Rate
On the cms.gov site at this URL for searching you can type in your HCPCS code (for the service) and MAC code (your location) and it will appear.
In my case, these values are:
90834for the HCPCS code1320201for the MAC code
Here’s the search:
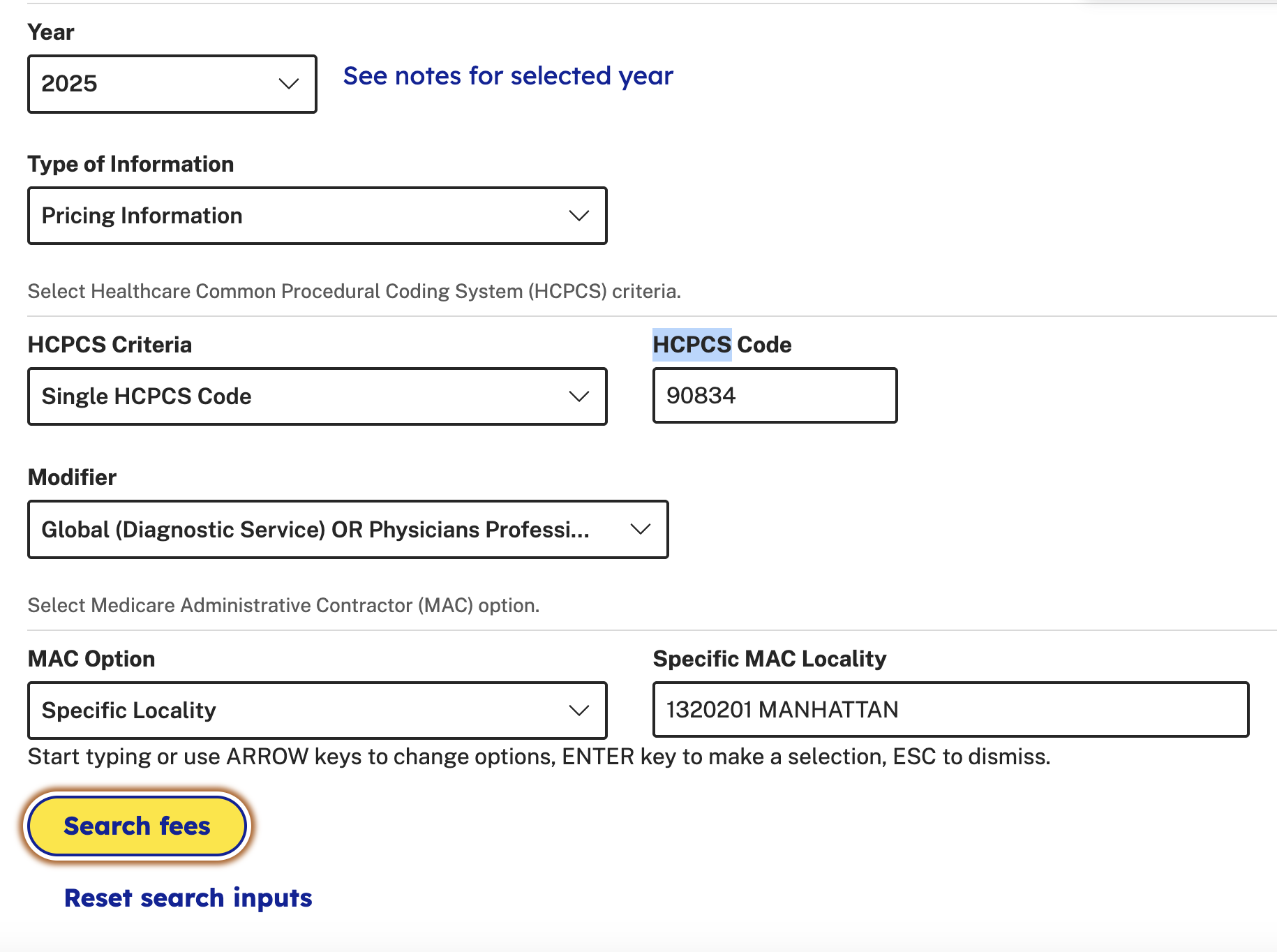
And here’s the result:
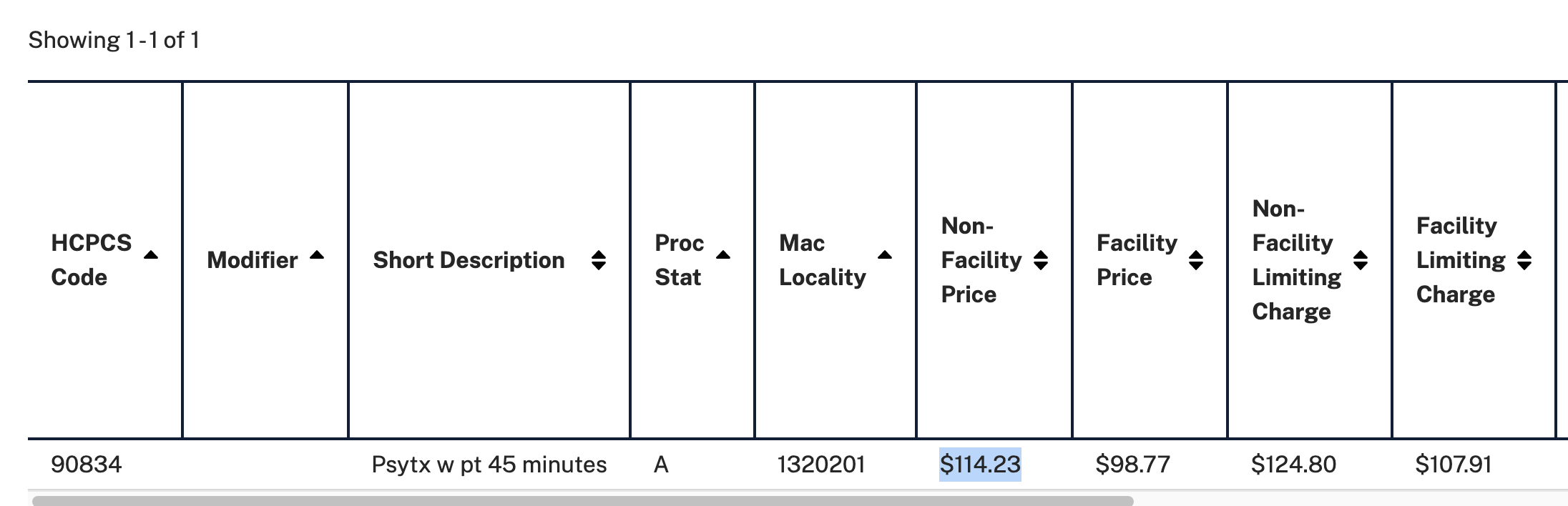
Taking the non-facility price (in-office visit) of $114.23 and multiplying by 140% you end up with $159.92. This is the amount that should have gone to my deductible.
That’s already sounding much better! Like a lower government number with a decent multiple applied.
When I called Aetna and spoke to a rep on the phone (today 5/8/2025) they confirmed the number I found. They said their internal system (for a publicly available number) also “calculated” that the reimbursement amount was exactly $159.92 down to the cent.
How could that be? The only excuse they managed to offer was “these rates change”. So maybe that explains the lower numbers in the previous claims?
However the number has been wrong every month in 2025 since February. And the wrong number has not changed ($119.94 has gone to my deductible for each appointment).
I’m also fairly certain the HCPCS codes change yearly (or possibly quarterly though that still wouldn’t explain this case). You can only search for them by year in the above link.
I think what changed was me calling with this information.
25% Reduction
If some group were interested in reimbursing a bit less, they may use the calculated number (the government number * the 140% multiple, which was $159.92) as a starting point.
Then, decide on some arbitrary percentage to reduce it by (let’s say an extremely obvious one, like 25%) to get a number that’s a bit lower, but close to the real one.
Let’s try doing that:
$159.92 * 0.75 = $119.94
What a strange coincidence! I almost wouldn’t believe it if the person on the phone didn’t confirm what I suspected the number should actually be. The adjustment was also done at a predictable percentage.
Result
So what will happen to the past claims? It didn’t sound like they would fix them.
I received a PDF in my email to write out and mail my complaint.
I didn’t receive any information that backs up the number they came up with.
It sounded like my submissions going forward will be fixed, but I received no confirmation of that either. Only a verbal confirmation the correct amount is what I found it to be.
Hopefully someone else reading this can save 25% on their out-of-network submissions with Aetna.
Caveat
I can’t see anything that says Aetna is required by law to pay 140% of the “Medicare Allowable Rate” for out-of-network medical claims.
I am simply investigating whether or not they actually stick to their own claims that they post publicly on their website.